Are You at Cancer Risk: Learn About BRCA Test, Gene Testing
How Cancer Happens
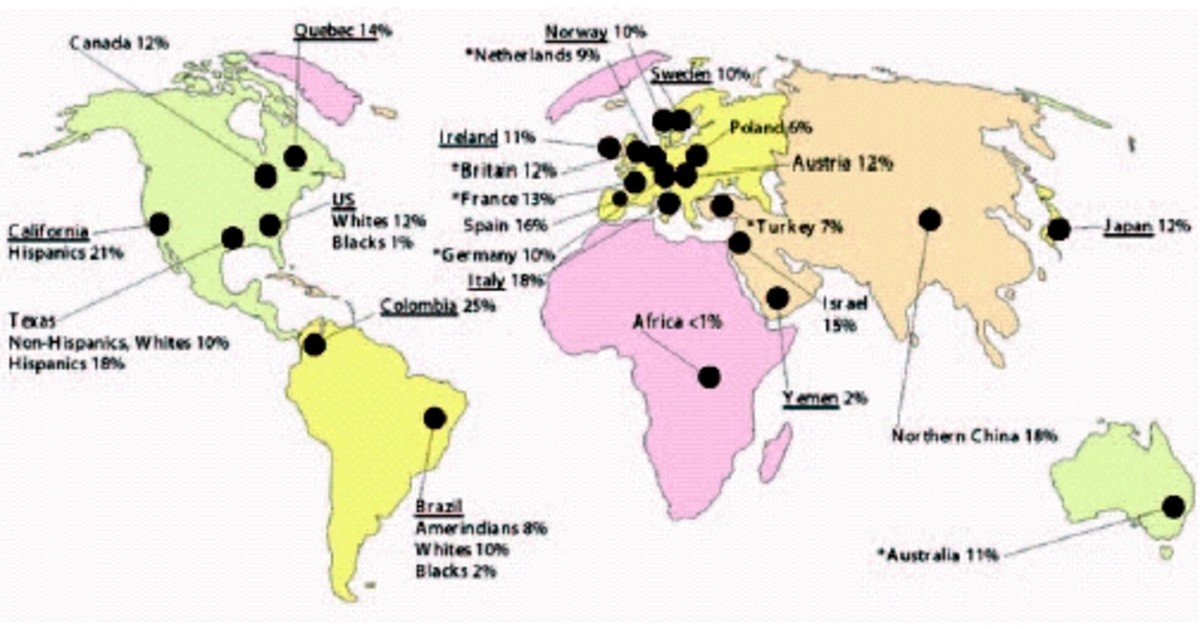
Breast cancer is a common disease that affects people of all races. It usually happens due to a combination of many different factors. About 1 in 8 women will be diagnosed with breast cancer in her lifetime and about 1 in 70 will get ovarian cancer. The majority of breast and ovarian cancers do not run in families.
Cancer happens when there are changes, called mutations, in the genes responsible for controlling cell growth. Genes are the instructions for how the body grows and functions. They determine traits like eye color and blood type; we have thousands of different genes in each of our cells. Mutations in genes cause the cells to grow out of control.
For most people who get cancer, the mutations in the genes happen at random and do not run in families. This is referred to as sporadic cancer. However, in some families, mutations that increase the risk for cancer can be passed down from one generation to the next. These type of cancers are referred to as hereditary cancers.
Testing for mutations in the BRCA genes requires a blood test.
Inherited Mutations
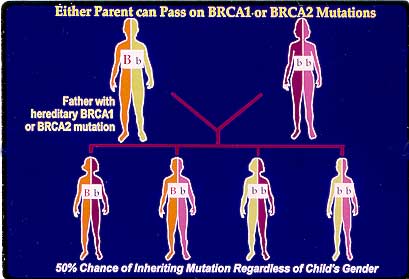
Approximately 5% to 10% of breast and ovarian cancers are associated with inherited mutations in cancer susceptibility genes. BRCA 1 and BRCA 2 account for the majority of families with hereditary patterns of breast and/or ovarian cancer. Mutations in the BRCA 1/2 genes are inherited in autosomal dominant fashion, meaning basically that offspring and siblings of known mutation carriers have a 50% chance of also having a mutation. Sex does not play a role here - both male and female carriers of BRCA1/2 mutations may pass these on to their offspring.
Factors that suggest a hereditary mutation in a family include:
- multiple family members with cancer
- early age of onset
- multiple cancers in the same individual
- occurrence or rare cancers
- Ashkenazi (Eastern European) Jewish heritage
Want to Read About My Breast Cancer Journey?
Cancer Risks in BRCA1/2 Mutation Carriers
Mutations in BRCA 1/2 lead to markedly increased lifetime risks for breast and ovarian cancer. Although the exact level of risk can vary among and within families, the current estimates of cancer risk for individuals who are positive for mutations in BRCA1 and BRCA2 are:
For BRCA1:
- risk of breast cancer (in women) up to 39% by age 50, up to 81% by age 80
- risk of second primary breast cancer (in women) between 40% to 64% by age 70; up to 20% risk of second primary breast cancer within 5 years of the first
- risk of ovarian cancer up to 21% by age 50, up to 54% by age 80
- risk of colon cancer is, in some families, slightly increased risk for men and women, approximately by 6% by age 70 (compared to 2% in the general population) has been observed
- risk of prostate cancer - some studies show an increased risk for males who carry a BRCA1 mutation of 8%-25% by age 70, compared to 14% in the general population.
For BRCA2:
- Risk of breast cancer (in women) up to 34% by age 50, up to 85% by age 80
- risk of breast cancer (in men) up to 7% by age 80
- risk of second breast cancer in women up to 50% by age 70, up to 12% risk of primary breast cancer within 5 years of the first
- risk of ovarian cancer up to 2% by age 50, up to 27% by age 80
- risk of other cancers (prostate, melanoma, pancreatic) may also be increased above the general population

Cancer Risk Management Options
For individuals who carry a mutation in BRCA1/2, the following management options are available. It must be stated that the effectiveness of increased cancer surveillance or other measures to reduce the risk of cancer in individuals who carry cancer susceptibility mutations has yet to be determined.
- Healthy lifestyle - a diet high in fiber and low in fat, regular exercise, alcohol in moderation only, avoid tobacco products. Although it is not yet known to what effect, if any, lifestyle factors may have on hereditary breast and ovarian cancer susceptibility, they may benefit many aspects of a person's overall health.
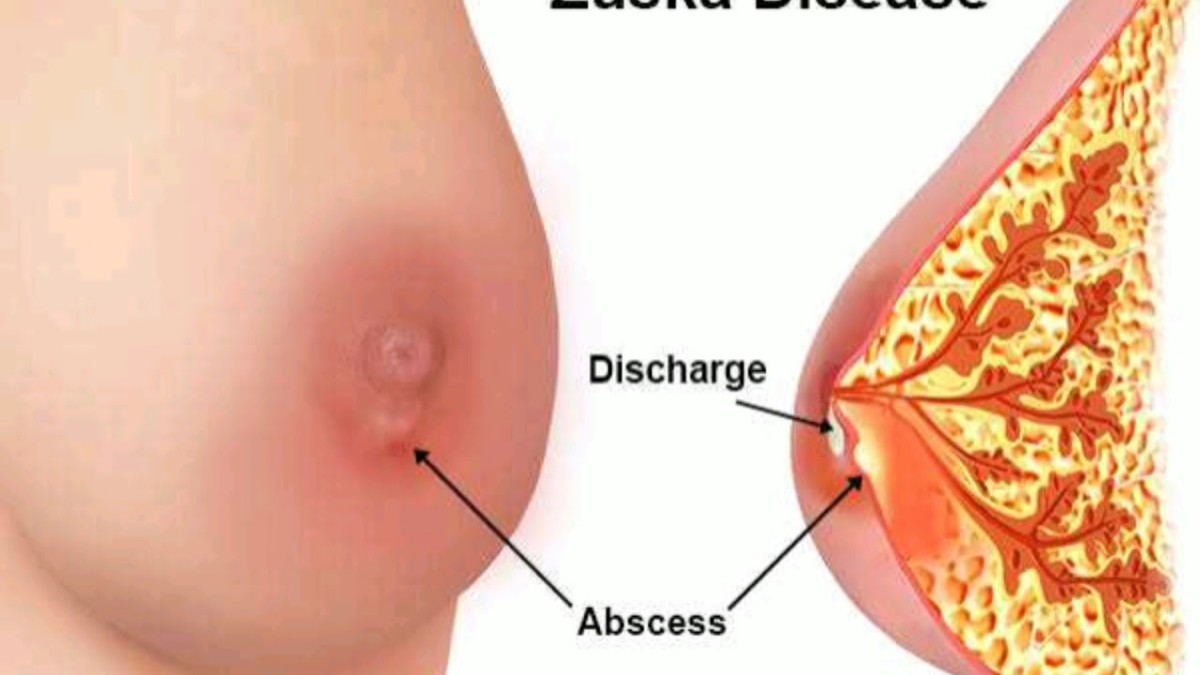
- Surveillance/screening - for breast cancer in women, mammograms, clinical breast exams and self-breast exams.
- For breast cancer in males - breast self-exam training and regular monthly practice, annual clinical breast exam, consider baseline mammogram.
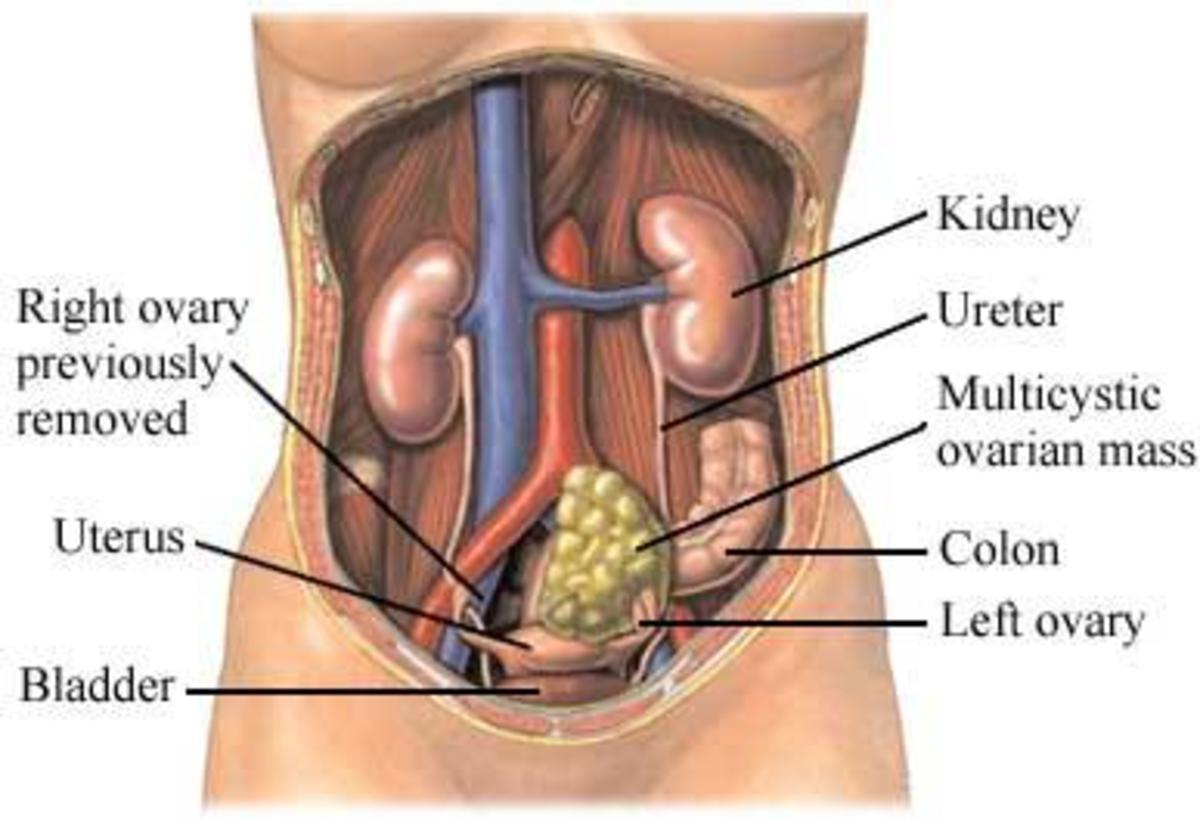
- For ovarian cancer - pelvic exams every 6 to 12 months, transvaginal ultrasound, and annual CA-125 blood test. Currently, however, there is no evidence to prove that these tests are effective in reducing ovarian cancer mortality.
- For prostate cancer - screening options include PSA blood test, digital rectal exam and transrectal ultrasound by an experienced physician. Men at high risk should discuss screening options with their doctor by age 40.
- For pancreatic cancer - reports indicate increased risk in families with BRCA2 mutations; however, there currently are no proven screening methods for pancreatic cancer.
- Risk reducing surgery (for breast cancer) - prophylactic mastectomy. Studies of the effect of risk reducing mastectomy in women with BRCA1/2 mutations report that the surgery decreases the risk of breast cancer by 90%.
- Risk reducing surgery (for ovarian cancer) - prophylactic salpingo-oopherectomy (removal of the ovaries and fallopian tubes). Studies of women with BRCA 1/2 mutations who underwent this procedure report a risk reduction in the range of 95% or more. Furthermore, this procedure performed on women before menopause would also reduce the risk of breast cancer.
- Chemoprevention (for breast cancer) - several chemotherapeutic agents such as Tamoxifen and Raloxifen may have a role in reducing risk of breast cancer in high-risk families.
- Chemoprevention (for ovarian cancer) - birth control pills reduce the risk in the general population. One study reports that this effect may also apply to carriers of BRCA 1/2 mutations, in whom the risk may be reduced by as much as 50%. However, one study of BRCA1 mutation carriers suggested that taking birth control pills before the age of 30 may increase their risk of breast cancer. Another study suggests that current low dose formulations do not increase the risk of breast cancer in mutation carriers.
Counseling Issues
It is recommended that carriers of BRCA mutations notify family members of her mutation status because there is a 50% probability - a 1 in 2 chance - for each of the carrier's first degree relatives (children, siblings, parents) to carry the same mutation. Males and females have the same chance of carrying and passing on these mutations, even if their cancer risks are different. They may choose to use the information to consider genetic counseling and BRCA 1/2 testing for themselves.
BRCA 1/2 mutations do not lead to childhood cancers, and there are no medical interventions available to minors, so genetic testing is only given to individuals over 18.
With the development of potential preventive strategies against cancer on the horizon, having this information may be crucial to the carrier's family members in accessing the most appropriate cancer risk management strategies.
Psychosocial Issues
The decision to take a blood test to determine if a person carries a BRCA mutation is very personal and can have complex, and sometimes unexpected, psychological and emotional distress about being at high risk for cancer. Consultation with a mental health expert may help a carrier to cope with these and other feelings. There are also a number of online support groups for women and men at risk, such as FORCE - Facing Our Risk of Cancer Empowered.
October is Breast Cancer Awareness Month

Related articles:
- Did My Cancer Save My Mom's Life?
- What I Learned From Cancer Treatment
- Breast Cancer Treatment - Things The Doctors Don't Tell You
- Breast Cancer Treatment - What Else They Don't Tell You
- Breast Cancer Treatment - Just Another Bump In The Road
- Breast Cancer Info - My Favorite Online Resources
- Chemotherapy Hair Loss : Products to Help